Kaiser Health News
The Unusual Way a Catholic Health System Is Wielding an Abortion Protest Law
Judy Lin
Wed, 15 Nov 2023 10:00:00 +0000
A Catholic hospital system is suing several California patients and their advocates because the patients allegedly refused to be discharged. The suits invoke a novel legal approach: accusing them of trespassing under a California law intended to stop anti-abortion protesters from blocking access to health facilities.
Dignity Health has filed three lawsuits in Sacramento County accusing patients of “commercial blockade” for refusing to vacate hospital beds even though the health care provider had deemed them medically and legally eligible to either go home or go to another facility. Dignity alleges the patients “unreasonably and unlawfully” refused discharge, disrupting its ability to serve others at a time when health facilities were overwhelmed by covid-19.
Relatives and advocates say the patients were exercising their right to be discharged to a facility that offered appropriate care and that they could afford, not simply sent home without the ability to take care of themselves.
The lawsuits, one of which is scheduled to begin trial proceedings Nov. 15, could set important precedents for both the use of the California commercial blockade statute to go after patients and their advocates and, more broadly, the handling of cases in which the hospital and patient can't agree on a plan for discharge.
The state's hospital lobby recently highlighted discharge delays as a growing problem costing the industry $2.9 billion a year. The California Hospital Association estimates at least 5,000 patients every day experience such delays, often in trying to identify skilled nursing facilities.
Patient advocates, who typically charge patients a fee to help them navigate the health care system, warn that a decision in favor of Dignity could chill their entire profession and give hospitals a new avenue to seek money from patients.
“It could be a watershed case if it goes in either direction,” said Tony Chicotel, senior staff attorney with the Berkeley-based California Advocates for Nursing Home Reform, who has worked on hospital discharge cases. “If it's a defense verdict, we'll know our laws are somewhat protective of patients. And if it's a plaintiff's verdict, patients around the state could be dumped and us advocates will have to figure out what we can talk about without getting sued.”
San Francisco-based Dignity Health, a tax-exempt organization with $9.5 billion in revenue, was founded by nuns to serve the sick and the poor. Spokesperson William Hodges said the health system doesn't comment on pending litigation.
A 68-year-old patient, Daphne Muehlendorf, who is blind, began suffering a series of seizures in 2021 and was in and out of the hospital. Each time she went home, her daughters say, her health declined, with slurred speech and the inability to carry a cup, despite receiving in-home physical therapy. By the time she entered the acute rehabilitation unit at Dignity's Mercy General Hospital in Sacramento, she had already applied for Medi-Cal, the state's Medicaid program, which covers the cost of nursing homes if the patient demonstrates both financial and medical need.
Dignity, which has not specified an amount it seeks in damages, contends in its lawsuit that doctors determined Muehlendorf was eligible to go home but the family refused for weeks while waiting for her Medi-Cal assisted living waiver to be approved. Once that came through, Muehlendorf was transferred to Bruceville Terrace, one of Dignity's skilled nursing facilities in Sacramento.
“I don't see what the case is and that's what's scary for me,” said one of Muehlendorf's two daughters, Terra Khan, about Dignity's legal argument. She is also being sued by Dignity. “I have no idea what's going to happen. I'm terrified.”
Dennis McPherson, the attorney representing Dignity, said the hospital made the decision to sue after serious deliberation. Muehlendorf “did cause a significant disruption,” McPherson said. “It took a lot more manpower and our unit was full. There were patients wait-listed who couldn't get into this unit.”
The family and their patient advocate, Carol Costa-Smith, who runs the company The Light for Seniors in San Diego, said it wasn't safe for Muehlendorf to return home and accused the hospital of delaying filing paperwork for Muehlendorf's Medi-Cal application. State and federal laws require hospitals to arrange care for patients who are likely to suffer adverse health consequences upon discharge, and patients have a right to appeal discharge decisions.
Likening themselves to tax advisers, independent advocates with legal, finance, and insurance backgrounds fill a cottage industry helping patients and their families navigate the health system and long-term care facilities, which often includes applying for Medi-Cal.
Costa-Smith, who charges each client $2,000 to $3,000 a year, said Dignity is trying to put patient advocates out of business so there is less pushback against hospital discharges and other decisions. “I'm the pit bull and I'm not going to let them do a home discharge if it's not safe,” she said.
Muehlendorf's trial is scheduled to begin this week.
Dignity's use of the commercial blockade law appears to be new. California lawmakers passed a bill in 1994 allowing civil claims against trespassers at health facilities, authored by then-Assembly member Jackie Speier, who recently retired from Congress and is now running for the San Mateo County Board of Supervisors. The legislature's analysis of the proposed bill from that time showed it was intended to dissuade anti-abortion protesters from blocking people entering or exiting health care facilities by threatening a lawsuit.
The analysis said it could also stop other disruptive activities such as excessive phone calls to tie up phone lines, the use of stink bombs to evacuate health facilities, and fake fire calls that prompt emergency evacuation. It was backed by the American College of Obstetricians and Gynecologists, California NOW, and Planned Parenthood Affiliates of California.
Anti-abortion groups opposed the bill, arguing “those who impede access in order to save babies should not be treated differently than those who might do so to save animals, or to block access to government buildings or bridges.” Opponents suggested that pro-choice groups could seek to exploit the bill for profit.
Patient advocates are alarmed by the Dignity lawsuits and say they have never heard of hospitals filing such claims. Dignity is also suing Craig Smedley, who operates Estate Advisory Group in Murrieta. According to a June 30, 2021, complaint, Smedley advised a patient at Mercy Hospital of Folsom “refusal to accept safe and lawful placement and be discharged” even though the patient had been medically eligible for discharge since May 9, 2021.
Dignity contends it lost money because the patient's insurance denied payment, and it accuses Smedley of directing the hospital to send her to a skilled nursing facility when doctors said she had no need for that level of care. Dignity has not specified an amount it seeks in damages. Smedley, who is defending himself, said disagreeing with a hospital's discharge plan was hardly a commercial blockade.
“I'm not chaining myself to the front door to prevent people from passing through to the hospital like an anti-abortion protester,” Smedley said. “I've never visited the hospital. I give advice by phone. My clients were the ones communicating with the hospital.”
Chicotel, the attorney with the nursing home reform group, said he did not believe Dignity's claims were supported by the law. Hospitals, he said, have a duty to discharge patients to a safe facility they can afford.
“In my experience, the Catholic hospitals are focused on the bottom line,” Chicotel said. “We see finances become much more important than the spiritual mission. I see that over and over again.”
McPherson argued that the commercial blockade law was written broadly to include any disruption to the normal functions of a health care facility that renders it temporarily or permanently unavailable.
“The outcome of the trial will dictate to the client what we're going to do with respect to the others,” he said. Dignity has filed a third lawsuit, against Costa-Smith and another client.
As a registered nurse who has worked for various hospitals, Khan believes she was doing what any person would do in advocating for a loved one. She said her mother, who once lived independently despite her disability, wouldn't have asked for help if she didn't really need it. “I know we moved through this honorably,” she said.
Khan is both troubled and comforted knowing that Dignity is going after other patients and patient advocates.
“It makes me feel like, OK, it wasn't that we did something wrong — there's something else at play that we're not privy to.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
——————————
By: Judy Lin
Title: The Unusual Way a Catholic Health System Is Wielding an Abortion Protest Law
Sourced From: kffhealthnews.org/news/article/catholic-hospitals-dignity-health-abortion-protest-law-discharge/
Published Date: Wed, 15 Nov 2023 10:00:00 +0000
Did you miss our previous article…
https://www.biloxinewsevents.com/facing-financial-ruin-as-costs-soar-for-elder-care/
Kaiser Health News
Millions Were Booted From Medicaid. The Insurers That Run It Gained Medicaid Revenue Anyway.
Phil Galewitz, KFF Health News
Fri, 26 Apr 2024 13:55:00 +0000
Private Medicaid health plans lost millions of members in the past year as pandemic protections that prohibited states from dropping anyone from the government program expired.
But despite Medicaid's unwinding, as it's known, at least two of the five largest publicly traded companies selling plans have continued to increase revenue from the program, according to their latest earnings reports.
“It's a very interesting paradox,” said Andy Schneider, a research professor at Georgetown University's McCourt School of Public Policy, of plans' Medicaid revenue increasing despite enrollment drops.
Medicaid, the state-federal health program for low-income and disabled people, is administered by states. But most people enrolled in the program get their health care through insurers contracted by states, including UnitedHealthcare, Centene, and Molina.
The companies persuaded states to pay them more money per Medicaid enrollee under the assumption that younger and healthier people were dropping out — presumably for Obamacare coverage or employer-based health insurance, or because they didn't see the need to get coverage — leaving behind an older and sicker population to cover, their executives have told investors.
Several of the companies reported that states have made midyear and retrospective changes in their payments to plans to account for the worsening health status of members.
In an earnings call with analysts on April 25, Molina Healthcare CEO Joe Zubretsky said 19 states increased their payment rates this year to adjust for sicker Medicaid enrollees. “States have been very responsive,” Zubretsky said. “We couldn't be more pleased with the way our state customers have responded to having rates be commensurate with normal cost trends and trends that have been influenced by the acuity shift.”
Health plans have faced much uncertainty during the Medicaid unwinding, as states began reassessing enrollees' eligibility and dropping those deemed no longer qualified or who lost coverage because of procedural errors. Before the unwinding, plans said they expected the overall risk profile of their members to go up because those remaining in the program would be sicker.
UnitedHealthcare, Centene, and Molina had Medicaid revenue increases ranging from 3% to 18% in 2023, according to KFF. The two other large Medicaid insurers, Elevance and CVS Health, do not break out Medicaid-specific revenue.
The Medicaid enrollment of the five companies collectively declined by about 10% from the end of March 2023 through the end of December 2023, from 44.2 million people to 39.9 million, KFF data shows.
In the first quarter of 2024, UnitedHealth's Medicaid revenue rose to $20.5 billion, up from $18.8 billion in the same quarter of 2023.
Molina on April 24 reported nearly $7.5 billion in Medicaid revenue in the first quarter of 2024, up from $6.3 billion in the same quarter a year earlier.
On April 26, Centene reported that its Medicaid enrollment fell 18.5% to 13.3 million in the first quarter of 2024 compared with the same period a year ago. The company's Medicaid revenue dipped 3% to $22.2 billion.
Unlike UnitedHealthcare, whose Medicaid enrollment fell to 7.7 million in March 2024 from 8.4 million a year prior, Molina's Medicaid enrollment rose in the first quarter of 2024 to 5.1 million from 4.8 million in March 2023. Molina's enrollment jump last year was partly a result of its having bought a Medicaid plan in Wisconsin and gained a new Medicaid contract in Iowa, the company said in its earnings news release.
Molina added 1 million members because states were prohibited from terminating Medicaid coverage during the pandemic. The company has lost 550,000 of those people during the unwinding and expects to lose an additional 50,000 by June.
About 90% of Molina Medicaid members have gone through the redetermination process, Zubretsky said.
The corporate giants also offset the enrollment losses by getting more Medicaid money from states, which they use to pass on higher payments to certain facilities or providers, Schneider said. By holding the money temporarily, the companies can count these “directed payments” as revenue.
Medicaid health plans were big winners during the pandemic after the federal government prohibited states from dropping people from the program, leading to a surge in enrollment to about 93 million Americans.
States made efforts to limit health plans' profits by clawing back some payments above certain thresholds, said Elizabeth Hinton, an associate director at KFF.
But once the prohibition on dropping Medicaid enrollees was lifted last spring, the plans faced uncertainty. It was unclear how many people would lose coverage or when it would happen. Since the unwinding began, more than 20 million people have been dropped from the rolls.
Medicaid enrollees' health care costs were lower during the pandemic, and some states decided to exclude pandemic-era cost data as they considered how to set payment rates for 2024. That provided yet another win for the Medicaid health plans.
Most states are expected to complete their Medicaid unwinding processes this year.
——————————
By: Phil Galewitz, KFF Health News
Title: Millions Were Booted From Medicaid. The Insurers That Run It Gained Medicaid Revenue Anyway.
Sourced From: kffhealthnews.org/news/article/medicaid-unwinding-insurer-revenue/
Published Date: Fri, 26 Apr 2024 13:55:00 +0000
Did you miss our previous article…
https://www.biloxinewsevents.com/california-is-investing-500m-in-therapy-apps-for-youth-advocates-fear-it-wont-pay-off/
Kaiser Health News
California Is Investing $500M in Therapy Apps for Youth. Advocates Fear It Won’t Pay Off.
Molly Castle Work
Fri, 26 Apr 2024 09:00:00 +0000
With little pomp, California launched two apps at the start of the year offering free behavioral health services to youths to help them cope with everything from living with anxiety to body acceptance.
Through their phones, young people and some caregivers can meet BrightLife Kids and Soluna coaches, some who specialize in peer support or substance use disorders, for roughly 30-minute virtual counseling sessions that are best suited to those with more mild needs, typically those without a clinical diagnosis. The apps also feature self-directed activities, such as white noise sessions, guided breathing, and videos of ocean waves to help users relax.
“We believe they're going to have not just great impact, but wide impact across California, especially in places where maybe it's not so easy to find an in-person behavioral health visit or the kind of coaching and supports that parents and young people need,” said Gov. Gavin Newsom's health secretary, Mark Ghaly, during the Jan. 16 announcement.
The apps represent one of the Democratic governor's major forays into health technology and come with four-year contracts valued at $498 million. California is believed to be the first state to offer a mental health app with free coaching to all young residents, according to the Department of Health Care Services, which operates the program.
However, the rollout has been slow. So slow that one of the companies has missed a deadline to make its app available on Android phones. Only about 15,000 of the state's 12.6 million children and young adults have signed up for the apps, and school counselors say they've never heard of them.
Advocates for youth question the wisdom of investing taxpayer dollars in two private companies. Social workers are concerned the companies' coaches won't properly identify youths who need referrals for clinical care. And the spending is drawing lawmaker scrutiny amid a state deficit pegged at as much as $73 billion.
An App for That
Newsom's administration says the apps fill a need for young Californians and their families to access professional telehealth for free, in multiple languages, and outside of standard 9-to-5 hours. It's part of Newsom's sweeping $4.7 billion master plan for kids' mental health, which was introduced in 2022 to increase access to mental health and substance use support services. In addition to launching virtual tools such as the teletherapy apps, the initiative is working to expand workforce capacity, especially in underserved areas.
“The reality is that we are rarely 6 feet away from our devices,” said Sohil Sud, director of Newsom's Children and Youth Behavioral Health Initiative. “The question is how we can leverage technology as a resource for all California youth and families, not in place of, but in addition to, other behavioral health services that are being developed and expanded.”
The virtual platforms come amid rising depression and suicide rates among youth and a shortage of mental health providers. Nearly half of California youths from the ages of 12 to 17 report having recently struggled with mental health issues, with nearly a third experiencing serious psychological distress, according to a 2021 study by the UCLA Center for Health Policy Research. These rates are even higher for multiracial youths and those from low-income families.
But those supporting youth mental health at the local level question whether the apps will move the needle on climbing depression and suicide rates.
“It's fair to applaud the state of California for aggressively seeking new tools,” said Alex Briscoe of California Children's Trust, a statewide initiative that, along with more than 100 local partners, works to improve the social and emotional health of children. “We just don't see it as fundamental. And we don't believe the youth mental health crisis will be solved by technology projects built by a professional class who don't share the lived experience of marginalized communities.”
The apps, BrightLife Kids and Soluna, are operated by two companies: Brightline, a 5-year-old venture capital-backed startup; and Kooth, a London-based publicly traded company that has experience in the U.K. and has also signed on some schools in Kentucky and Pennsylvania and a health plan in Illinois. In the first five months of Kooth's Pennsylvania pilot, 6% of students who had access to the app signed up.
Brightline and Kooth represent a growing number of health tech firms seeking to profit in this space. They beat out dozens of other bidders including international consulting companies and other youth telehealth platforms that had already snapped up contracts in California.
Although the service is intended to be free with no insurance requirement, Brightline's app, BrightLife Kids, is folded into and only accessible through the company's main app, which asks for insurance information and directs users to paid licensed counseling options alongside the free coaching. After KFF Health News questioned why the free coaching was advertised below paid options, Brightline reordered the page so that, even if a child has high-acuity needs, free coaching shows up first.
The apps take an expansive view of behavioral health, making the tools available to all California youth under age 26 as well as caregivers of babies, toddlers, and children 12 and under. When KFF Health News asked to speak with an app user, Brightline connected a reporter with a mother whose 3-year-old daughter was learning to sleep on her own.
‘It's Like Crickets'
Despite being months into the launch and having millions in marketing funds, the companies don't have a definitive rollout timeline. Brightline said it hopes to have deployed teams across the state to present the tools in person by midyear. Kooth said developing a strategy to hit every school would be “the main focus for this calendar year.”
“It's a big state — 58 counties,” Bob McCullough of Kooth said. “It'll take us a while to get to all of them.”
Brightline's contract states that the company was required to launch downloadable apps for iOS and Android phones by January, but so far BrightLife Kids is available only on Apple phones. Brightline said it's aiming to launch the Android version over the summer.
“Nobody's really done anything like this at this magnitude, I think, in the U.S. before,” said Naomi Allen, a co-founder and the CEO of Brightline. “We're very much in the early innings. We're already learning a lot.”
The contracts, obtained by KFF Health News through a records request, show the companies operating the two apps could earn as much as $498 million through the contract term, which ends in June 2027, months after Newsom is set to leave office. And the state is spending hundreds of millions more on Newsom's virtual behavioral health strategy. The state said it aims to make the apps available long-term, depending on usage.
The state said 15,000 people signed up in the first three months. When KFF Health News asked how many of those users actively engaged with the app, it declined to say, noting that data would be released this summer.
KFF Health News reached out to nearly a dozen California mental health professionals and youths. None of them were aware of the apps.
“I'm not hearing anything,” said Loretta Whitson, executive director of the California Association of School Counselors. “It's like crickets.”
Whitson said she doesn't think the apps are on “anyone's” radar in schools, and she doesn't know of any schools that are actively advertising them. Brightline will be presenting its tool to the counselor association in May, but Whitson said the company didn't reach out to plan the meeting; she did.
Concern Over Referrals
Whitson isn't comfortable promoting the apps just yet. Although both companies said they have a clinical team on staff to assist, Whitson said she's concerned that the coaches, who aren't all licensed therapists, won't have the training to detect when users need more help and refer them to clinical care.
This sentiment was echoed by other school-based social workers, who also noted the apps' duplicative nature — in some counties, like Los Angeles, youths can access free virtual counseling sessions through Hazel Health, a for-profit company. Nonprofits, too, have entered this space. For example, Teen Line, a peer-to-peer hotline operated by Southern California-based Didi Hirsch Mental Health Services, is free nationwide.
While the state is also funneling money to the schools as part of Newsom's master plan, students and school-based mental health professionals voiced confusion at the large app investment when, in many school districts, few in-person counseling roles exist, and in some cases are dwindling.
Kelly Merchant, a student at College of the Desert in Palm Desert, noted that it can be hard to access in-person therapy at her school. She believes the community college, which has about 15,000 students, has only one full-time counselor and one part-time bilingual counselor. She and several students interviewed by KFF Health News said they appreciated having engaging content on their phone and the ability to speak to a coach, but all said they'd prefer in-person therapy.
“There are a lot of people who are seeking therapy, and people close to me that I know. But their insurances are taking forever, and they're on the waitlist,” Merchant said. “And, like, you're seeing all these people struggle.”
Fiscal conservatives question whether the money could be spent more effectively, like to bolster county efforts and existing youth behavioral health programs.
Republican state Sen. Roger Niello, vice chair of the Senate Budget and Fiscal Review Committee, noted that California is forecasted to face deficits for the next three years, and taxpayer watchdogs worry the apps might cost even more in the long run.
“What starts as a small financial commitment can become uncontrollable expenses down the road,” said Susan Shelley of the Howard Jarvis Taxpayers Association.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
——————————
By: Molly Castle Work
Title: California Is Investing $500M in Therapy Apps for Youth. Advocates Fear It Won't Pay Off.
Sourced From: kffhealthnews.org/news/article/california-youth-teletherapy-apps-rollout-slow/
Published Date: Fri, 26 Apr 2024 09:00:00 +0000
Kaiser Health News
KFF Health News’ ‘What the Health?’: Abortion — Again — At the Supreme Court
Wed, 24 Apr 2024 20:30:00 +0000
The Host
Julie Rovner
KFF Health News
Julie Rovner is chief Washington correspondent and host of KFF Health News' weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Some justices suggested the Supreme Court had said its piece on abortion law when it overturned Roe v. Wade in 2022. This term, however, the court has agreed to review another abortion case. At issue is whether a federal law requiring emergency care in hospitals overrides Idaho's near-total abortion ban. A decision is expected by summer.
Meanwhile, the Centers for Medicare & Medicaid finalized the first-ever minimum staffing requirements for nursing homes participating in the programs. But the industry argues that there are not enough workers to hire to meet the standards.
This week's panelists are Julie Rovner of KFF Health News, Joanne Kenen of the Johns Hopkins University's nursing and public health schools and Politico Magazine, Tami Luhby of CNN, and Alice Miranda Ollstein of Politico.
Panelists
Joanne Kenen
Johns Hopkins University and Politico
Tami Luhby
CNN
Alice Miranda Ollstein
Politico
Among the takeaways from this week's episode:
- This week's Supreme Court hearing on emergency abortion care in Idaho was the first challenge to a state's abortion ban since the overturn of the constitutional right to an abortion. Unlike previous abortion cases, this one focused on the everyday impacts of bans on abortion care — cases in which pregnant patients experienced medical emergencies.
- Establishment medical groups and doctors themselves are getting more vocal and active as states set laws on abortion access. In a departure from earlier political moments, some major medical groups are campaigning on state ballot measures.
- Medicaid officials this week finalized new rules intended to more closely regulate managed-care plans that enroll Medicaid patients. The rules are intended to ensure, among other things, that patients have prompt access to needed primary care doctors and specialists.
- Also this week, the Federal Trade Commission voted to ban most “noncompete” clauses in employment contracts. Such language has become common in health care and prevents not just doctors but other health workers from changing jobs — often forcing those workers to move or commute to leave a position. Business interests are already suing to block the new rules, claiming they would be too expensive and risk the loss of proprietary information to competitors.
- The fallout from the cyberattack of Change Healthcare continues, as yet another group is demanding ransom from UnitedHealth Group, Change's owner. UnitedHealth said in a statement this week that the records of “a substantial portion of America” may be involved in the breach.
Plus for “extra credit” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: NBC News' “Women Are Less Likely To Die When Treated by Female Doctors, Study Suggests,” by Liz Szabo.
Alice Miranda Ollstein: States Newsroom's “Loss of Federal Protection in Idaho Spurs Pregnant Patients To Plan for Emergency Air Transport,” by Kelcie Moseley-Morris.
Tami Luhby: The Associated Press' “Mississippi Lawmakers Haggle Over Possible Medicaid Expansion as Their Legislative Session Nears End,” by Emily Wagster Pettus.
Joanne Kenen: States Newsroom's “Missouri Prison Agency To Pay $60K for Sunshine Law Violations Over Inmate Death Records,” by Rudi Keller.
Also mentioned on this week's podcast:
- American Economic Review's “Is There Too Little Antitrust Enforcement in the U.S. Hospital Sector?” by Zarek Brot-Goldberg, Zack Cooper, Stuart Craig, and Lev Klarnet.
- KFF Health News' “Medical Providers Still Grappling With UnitedHealth Cyberattack: ‘More Devastating Than Covid,” by Samantha Liss.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KFF Health News' “What the Health?” on Spotify, Apple Podcasts, Pocket Casts, or wherever you listen to podcasts.
——————————
Title: KFF Health News' ‘What the Health?': Abortion — Again — At the Supreme Court
Sourced From: kffhealthnews.org/news/podcast/what-the-health-344-abortion-supreme-court-april-25-2024/
Published Date: Wed, 24 Apr 2024 20:30:00 +0000
Did you miss our previous article…
https://www.biloxinewsevents.com/mandatory-reporting-laws-meant-to-protect-children-get-another-look/
-
Local News3 days ago
Sister of Mississippi man who died after police pulled him from car rejects lawsuit settlement
-
Mississippi Today3 days ago
At Lake High School in Scott County, the Un-Team will never be forgotten
-
Mississippi News1 day ago
One injured in Mississippi officer-involved shooting after chase
-
Mississippi News6 days ago
Cicadas expected to takeover north Mississippi counties soon
-
Mississippi News5 days ago
Viewers make allegations against Hatley teacher, school district releases statement – Home – WCBI TV
-
Mississippi Today11 hours ago
On this day in 1951
-
Mississippi News Video4 days ago
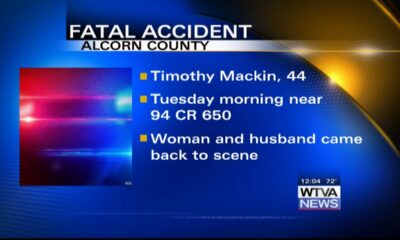
Vehicle struck and killed man lying in the road, Alcorn County sheriff says
-
Mississippi Today6 days ago
On this day in 1892