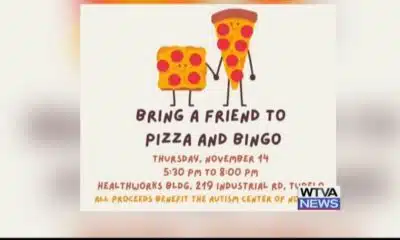

www.youtube.com – WTVA 9 News – 2024-11-07 15:42:38 SUMMARY: The Autism Center of North Mississippi, led by Executive Director Melinda Tidwell, is hosting a fundraiser called...


Read the full article The post Mississippi legislative leaders advocate Medicaid expansion, heading to conflict with the governor appeared first on www.wxxv25.com


Read the full article The post Mississippi legislative leaders advocate Medicaid expansion, heading to conflict with the governor appeared first on www.wjtv.com


Read the full article The post Mississippi legislative leaders advocate Medicaid expansion, heading to conflict with the governor appeared first on www.supertalk.fm


Read the full article The post In Montana, Conservative Groups See Chance To Kill Medicaid Expansion appeared first on kffhealthnews.org


Read the full article The post For People With Opioid Addiction, Medicaid ‘Unwinding’ Raises the Stakes appeared first on kffhealthnews.org


www.youtube.com – WJTV 12 News – 2024-10-28 12:13:09 SUMMARY: A recent report by the Mississippi state auditor highlighted millions in misspent funds across 13 state agencies,...


www.youtube.com – KHOU 11 – 2024-10-25 18:13:07 SUMMARY: Starting November 1st, MD Anderson Cancer Center will no longer accept Blue Cross Blue Shield Managed Medicare Advantage...


www.youtube.com – WTOK-TV – 2024-10-24 09:11:31 SUMMARY: Mr. William Vickers, a volunteer from the State Health Insurance Assistance Program (SHIP) through United Way, offers valuable support...

www.youtube.com – FOX 4 Dallas-Fort Worth – 2024-10-22 18:01:55 SUMMARY: Starting November 1, Texas hospitals will be required to ask patients about their citizenship status, as...