Kaiser Health News
The ‘Unwinding’ of Medicaid
by
Thu, 06 Apr 2023 18:50:00 +0000
The Host
Julie Rovner
KHN
Julie Rovner is chief Washington correspondent and host of KHN's weekly health policy news podcast, “What the Health?” A noted expert on health policy issues, Julie is the author of the critically praised reference book “Health Care Politics and Policy A to Z,” now in its third edition.
Several states have begun the herculean task of redetermining how many of an estimated 85 million Americans currently receiving health coverage through the Medicaid program are still eligible. To receive federal covid-19 relief funds, states were required to keep enrollees covered during the pandemic. As many as 15 million people could be struck from the program's rolls — many of whom are still eligible, or are eligible for other programs and need to be steered to them.
Meanwhile, the trustees of the Medicare program report that its Hospital Insurance Trust Fund should remain solvent until 2031, three years longer than it projected last year. That allows lawmakers to continue to put off what are likely to be politically unpleasant decisions, although they will eventually have to deal with Medicare's underlying financial woes (and those of Social Security).
Panelists
Alice Miranda Ollstein
Politico
Amy Goldstein
The Washington Post
Rachel Roubein
The Washington Post
Among the takeaways from this week's episode:
- The Medicaid “unwinding” is likely to strip health coverage not just from millions of people who are no longer eligible for the program, but also from millions of people who still are. States are supposed to take their time reevaluating eligibility, but some are rushing to disenroll people.
- Another complication in an already complicated task is that many Medicaid workers hired during the pandemic have never actually redetermined Medicaid eligibility for anyone, because states had been required to keep people who qualified on the program.
- Grimly, some of the extra years of solvency gained in the Medicare Hospital Insurance Trust Fund are a result of pandemic deaths in the 65-and-older population.
- The Department of Health and Human Services has issued payment rules for Medicare Advantage Plans for 2024. The agency ended up conceding at least somewhat to private plans that for years have been receiving more than they should have from the U.S. Treasury. The new rules will work to shrink those overpayments going forward, but not try to recoup those from years past.
- The situation with “first-dollar coverage” of preventive services by commercial health plans is becoming a bit clearer following last week's decision in Texas that part of the Affordable Care Act's preventive services mandate is unconstitutional. Judge Reed O'Connor (who in 2018 ruled the entire health law unconstitutional) issued a nationwide stay on coverage requirements from the U.S. Preventive Services Task Force, saying it is a volunteer organization not subject to the oversight of the Health and Human Services secretary. The federal government is already appealing that ruling.
- But O'Connor's decision is not quite as sweeping as first thought. He banned required coverage only of the task force's recommendations made after March 23, 2010 — the day the ACA was signed into law. Earlier recommendations stand. O'Connor also did not strike preventive services recommended by the Health Resources and Services Administration and the Centers for Disease Control and Prevention's Advisory Committee on Immunization Practices, since those agencies are overseen by an official appointed by the president and confirmed by the Senate.
- In abortion news, the liberal candidate for a Supreme Court seat in Wisconsin, Janet Protasiewicz, defeated her conservative opponent to switch the majority on the court from 4-3 conservative to 4-3 liberal. That ideological shift is likely to preserve abortion rights in the state, and possibly stem the ability of the GOP legislature to continue to draw maps that favor Republicans.
- Meanwhile, states in the South are continuing to pull back on abortion access. The Florida legislature is moving rapidly on a bill that would ban the procedure after six weeks of pregnancy, while in North Carolina, a single legislator's switch from Democrat to Republican has given the latter a supermajority in the legislature large enough to override any veto of the Democratic governor, Roy Cooper.
Also this week, Rovner interviews Daniel Chang, who reported and wrote the latest KHN-NPR “Bill of the Month” feature about a child who had a medical bill sent to collections before he started to learn to read. If you have an outrageous or exorbitant medical bill you want to share with us, you can do that here.
Plus, for “extra credit,” the panelists suggest health policy stories they read this week that they think you should read, too:
Julie Rovner: New York Magazine's “The Shared Anti-Trans and Anti-Abortion Playbook,” by Irin Carmon.
Alice Miranda Ollstein: The Los Angeles Times' “Horrifying Stories of Women Chased Down by the LAPD Abortion Squad Before Roe vs. Wade,” by Brittny Mejia.
Rachel Roubein: KHN's “‘Hard to Get Sober Young': Inside One of the Country's Few Recovery High Schools,” by Stephanie Daniel of KUNC.
Amy Goldstein: The Washington Post's “After Decades Under a Virus's Shadow, He Now Lives Free of HIV,” by Mark Johnson.
Also mentioned in this week's podcast:
- Stat's “Denied by AI: How Medicare Advantage Plans Use Algorithms to Cut Off Care for Seniors in Need,” by Casey Ross and Bob Herman.
- ProPublica's “How Cigna Saves Millions by Having Its Doctors Reject Claims Without Reading Them,” by Patrick Rucker, Maya Miller, and David Armstrong.
- The Atlantic's “There's No Such Thing as a Casual Interaction With Your Doctor Anymore,” by Zoya Qureshi.
- Politico's “Democrats Want to Restore Roe. They're Divided on Whether to Go Even Further,” by Alice Miranda Ollstein and Megan Messerly.
Credits
Francis Ying
Audio producer
Emmarie Huetteman
Editor
To hear all our podcasts, click here.
And subscribe to KHN's What the Health? on Spotify, Apple Podcasts, Stitcher, Pocket Casts, or wherever you listen to podcasts.
Title: The ‘Unwinding' of Medicaid
Sourced From: khn.org/news/podcast/podcast-khn-what-the-health-292-medicaid-unwinding-april-6-2023/
Published Date: Thu, 06 Apr 2023 18:50:00 +0000
Kaiser Health News
Exposed to Agent Orange at US Bases, Veterans Face Cancer Without VA Compensation
Hannah Norman, KFF Health News and Patricia Kime
Mon, 29 Apr 2024 09:00:00 +0000
As a young GI at Fort Ord in Monterey County, California, Dean Osborn spent much of his time in the oceanside woodlands, training on soil and guzzling water from streams and aquifers now known to be contaminated with cancer-causing pollutants.
“They were marching the snot out of us,” he said, recalling his year and a half stationed on the base, from 1979 to 1980. He also remembers, not so fondly, the poison oak pervasive across the 28,000-acre installation that closed in 1994. He went on sick call at least three times because of the overwhelmingly itchy rash.
Mounting evidence shows that as far back as the 1950s, in an effort to kill the ubiquitous poison oak and other weeds at the Army base, the military experimented with and sprayed the powerful herbicide combination known colloquially as Agent Orange.
While the U.S. military used the herbicide to defoliate the dense jungles of Vietnam and adjoining countries, it was contaminating the land and waters of coastal California with the same chemicals, according to documents.
The Defense Department has publicly acknowledged that during the Vietnam War era it stored Agent Orange at the Naval Construction Battalion Center in Gulfport, Mississippi, and the former Kelly Air Force Base in Texas, and tested it at Florida's Eglin Air Force Base.
According to the Government Accountability Office, however, the Pentagon's list of sites where herbicides were tested went more than a decade without being updated and lacked specificity. GAO analysts described the list in 2018 as “inaccurate and incomplete.”
Fort Ord was not included. It is among about four dozen bases that the government has excluded but where Pat Elder, an environmental activist, said he has documented the use or storage of Agent Orange.
According to a 1956 article in the journal The Military Engineer, the use of Agent Orange herbicides at Fort Ord led to a “drastic reduction in trainee dermatitis casualties.”
“In training areas, such as Fort Ord, where poison oak has been extremely troublesome to military personnel, a well-organized chemical war has been waged against this woody plant pest,” the article noted.
Other documents, including a report by an Army agronomist as well as documents related to hazardous material cleanups, point to the use of Agent Orange at the sprawling base that 1.5 million service members cycled through from 1917 to 1994.
‘The Most Toxic Chemical'
Agent Orange is a 50-50 mixture of two ingredients, known as 2,4-D and 2,4,5-T. Herbicides with the same chemical structure slightly modified were available off the shelf, sold commercially in massive amounts, and used at practically every base in the U.S., said Gerson Smoger, a lawyer who argued before the Supreme Court for Vietnam veterans to have the right to sue Agent Orange manufacturers. The combo was also used by farmers, forest workers, and other civilians across the country.
The chemical 2,4,5-T contains the dioxin 2,3,7,8-tetrachlorodibenzo-p-dioxin or TCDD, a known carcinogen linked to several cancers, chronic conditions and birth defects. A recent Brown University study tied Agent Orange exposure to brain tissue damage similar to that caused by Alzheimer's. Acknowledging its harm to human health, the Environmental Protection Agency banned the use of 2,4,5-T in the U.S. in 1979. Still, the other weed killer, 2,4-D is sold off-the-shelf today.
“The bottom line is TCDD is the most toxic chemical that man has ever made,” Smoger said.
For years, the Department of Veteran Affairs has provided vets who served in Vietnam disability compensation for diseases considered to be connected to exposure to Agent Orange for military use from 1962 to 1975.
Decades after Osborn's military service, the 68-year-old veteran, who never served in Vietnam, has battled one health crisis after another: a spot on his left lung and kidney, hypothyroidism, and prostate cancer, an illness that has been tied to Agent Orange exposure.
He says many of his old buddies from Fort Ord are sick as well.
“Now we have cancers that we didn't deserve,” Osborn said.
The VA considers prostate cancer a “presumptive condition” for Agent Orange disability compensation, acknowledging that those who served in specific locations were likely exposed and that their illnesses are tied to their military service. The designation expedites affected veterans' claims.
But when Osborn requested his benefits, he was denied. The letter said the cancer was “more likely due to your age,” not military service.
“This didn't happen because of my age. This is happening because we were stationed in the places that were being sprayed and contaminated,” he said.
Studies show that diseases caused by environmental factors can take years to emerge. And to make things more perplexing for veterans stationed at Fort Ord, contamination from other harmful chemicals, like the industrial cleaner trichloroethylene, have been well documented on the former base, landing it on the EPA's Superfund site list in 1990.
“We typically expect to see the effect years down the line,” said Lawrence Liu, a doctor at City of Hope Comprehensive Cancer Center who has studied Agent Orange. “Carcinogens have additive effects.”
In February, the VA proposed a rule that for the first time would allow compensation to veterans for Agent Orange exposure at 17 U.S. bases in a dozen states where the herbicide was tested, used, or stored.
Fort Ord is not on that list either, because the VA's list is based on the Defense Department's 2019 update.
“It's a very tricky question,” Smoger said, emphasizing how widely the herbicides were used both at military bases and by civilians for similar purposes. “On one hand, we were service. We were exposed. On the other hand, why are you different from the people across the road that are privately using it?”
The VA says that it based its proposed rule on information provided by the Defense Department.
“DoD's review found no documentation of herbicide use, testing or storage at Fort Ord. Therefore, VA does not have sufficient evidence to extend a presumption of exposure to herbicides based on service at Fort Ord at this time,” VA press secretary Terrence Hayes said in an email.
The Documentation
Yet environmental activist Elder, with help from toxic and remediation specialist Denise Trabbic-Pointer and former VA physician Kyle Horton, compiled seven documents showing otherwise. They include a journal article, the agronomist report, and cleanup-related documents as recent as 1995 — all pointing to widespread herbicide use and experimentation as well as lasting contamination at the base.
Though the documents do not call the herbicide by its colorful nickname, they routinely cite the combination of 2,4-D and 2,4,5-T. A “hazardous waste minimization assessment” dated 1991 reported 80,000 pounds of herbicides used annually at Fort Ord. It separately lists 2,4,5-T as a product for which “substitutions are necessary to minimize the environmental impacts.”
The poison oak “control program” started in 1951, according to a report by Army agronomist Floyd Otter, four years before the U.S. deepened its involvement in Vietnam. Otter detailed the use of these chemicals alone and in combination with diesel oil or other compounds, at rates generally between “one to two gallons of liquid herbicide” per acre.
“In conclusion, we are fairly well satisfied with the methods,” Otter wrote, noting he was interested in “any way in which costs can be lowered or quicker kill obtained.”
An article published in California Agriculture more than a decade later includes before and after photos showing the effectiveness of chemical brush control used in a live-oak woodland at Fort Ord, again citing both chemicals in Agent Orange. The Defense Department did not respond to questions sent April 10 about the contamination or say when the Army stopped using 2,4,5-T at Fort Ord.
“What's most compelling about Fort Ord is it was actually used for the same purpose it was used for in Vietnam — to kill plants — not just storing it,” said Julie Akey, a former Army linguist who worked at the base in the 1990s and later developed the rare blood cancer multiple myeloma.
Akey, who also worked with Elder, runs a Facebook group and keeps a list of people stationed on the base who later were diagnosed with cancer and other illnesses. So far, she has tallied more than 1,400 former Fort Ord residents who became sick.
Elder's findings have galvanized the group to speak up during a public comment period for the VA's proposed rule. Of 546 comments, 67 are from veterans and others urging the inclusion of Fort Ord. Hundreds of others have written in regarding the use of Agent Orange and other chemicals at their bases.
While the herbicide itself sticks around for only a short time, the contaminant TCDD can linger in sediment for decades, said Kenneth Olson, a professor emeritus of soil science at the University of Illinois Urbana-Champaign.
A 1995 report from the Army's Sacramento Corps of Engineers, which documented chemicals detected in the soil at Fort Ord, found levels of TCDD at 3.5 parts per trillion, more than double the remediation goal at the time of 1.2 ppt. Olson calls the evidence convincing.
“It clearly supports the fact that 2,4,5-T with unknown amounts of dioxin TCDD was applied on the Fort Ord grounds and border fences,” Olson said. “Some military and civilian personnel would have been exposed.”
The Department of Defense has described the Agent Orange used in Vietnam as a “tactical herbicide,” more concentrated than what was commercially available in the U.S. But Olson said his research suggests that even if the grounds maintenance crew used commercial versions of 2,4,5-T, which was available in the federal supply catalog, the soldiers would have been exposed to the dioxin TCDD.
The half dozen veterans who spoke with KFF Health News said they want the military to take responsibility.
The Pentagon did not respond to questions regarding the upkeep of the list or the process for adding locations.
In the meantime, the Agency for Toxic Substances and Disease Registry is studying potential chemical exposure among people who worked and lived on Fort Ord between 1985 and 1994. However, the agency is evaluating drinking water for contaminants such as trichloroethylene and not contamination or pollution from other chemicals such as Agent Orange or those found in firefighting foams.
Other veterans are frustrated by the VA's long process to recognize their illnesses and believe they were sickened by exposure at Fort Ord.
“Until Fort Ord is recognized by the VA as a presumptive site, it's probably going to be a long, difficult struggle to get some kind of compensation,” said Mike Duris, a 72-year-old veteran diagnosed with prostate cancer four years ago who ultimately underwent surgery.
Like so many others, he wonders about the connection to his training at Fort Ord in the early '70s — drinking the contaminated water and marching, crawling, and digging holes in the dirt.
“Often, where there is smoke, there's fire,” Duris said.
——————————
By: Hannah Norman, KFF Health News and Patricia Kime
Title: Exposed to Agent Orange at US Bases, Veterans Face Cancer Without VA Compensation
Sourced From: kffhealthnews.org/news/article/agent-orange-us-bases-veterans-face-cancer-without-va-compensation/
Published Date: Mon, 29 Apr 2024 09:00:00 +0000
Did you miss our previous article…
https://www.biloxinewsevents.com/millions-were-booted-from-medicaid-the-insurers-that-run-it-gained-medicaid-revenue-anyway/
Kaiser Health News
Millions Were Booted From Medicaid. The Insurers That Run It Gained Medicaid Revenue Anyway.
Phil Galewitz, KFF Health News
Fri, 26 Apr 2024 13:55:00 +0000
Private Medicaid health plans lost millions of members in the past year as pandemic protections that prohibited states from dropping anyone from the government program expired.
But despite Medicaid's unwinding, as it's known, at least two of the five largest publicly traded companies selling plans have continued to increase revenue from the program, according to their latest earnings reports.
“It's a very interesting paradox,” said Andy Schneider, a research professor at Georgetown University's McCourt School of Public Policy, of plans' Medicaid revenue increasing despite enrollment drops.
Medicaid, the state-federal health program for low-income and disabled people, is administered by states. But most people enrolled in the program get their health care through insurers contracted by states, including UnitedHealthcare, Centene, and Molina.
The companies persuaded states to pay them more money per Medicaid enrollee under the assumption that younger and healthier people were dropping out — presumably for Obamacare coverage or employer-based health insurance, or because they didn't see the need to get coverage — leaving behind an older and sicker population to cover, their executives have told investors.
Several of the companies reported that states have made midyear and retrospective changes in their payments to plans to account for the worsening health status of members.
In an earnings call with analysts on April 25, Molina Healthcare CEO Joe Zubretsky said 19 states increased their payment rates this year to adjust for sicker Medicaid enrollees. “States have been very responsive,” Zubretsky said. “We couldn't be more pleased with the way our state customers have responded to having rates be commensurate with normal cost trends and trends that have been influenced by the acuity shift.”
Health plans have faced much uncertainty during the Medicaid unwinding, as states began reassessing enrollees' eligibility and dropping those deemed no longer qualified or who lost coverage because of procedural errors. Before the unwinding, plans said they expected the overall risk profile of their members to go up because those remaining in the program would be sicker.
UnitedHealthcare, Centene, and Molina had Medicaid revenue increases ranging from 3% to 18% in 2023, according to KFF. The two other large Medicaid insurers, Elevance and CVS Health, do not break out Medicaid-specific revenue.
The Medicaid enrollment of the five companies collectively declined by about 10% from the end of March 2023 through the end of December 2023, from 44.2 million people to 39.9 million, KFF data shows.
In the first quarter of 2024, UnitedHealth's Medicaid revenue rose to $20.5 billion, up from $18.8 billion in the same quarter of 2023.
Molina on April 24 reported nearly $7.5 billion in Medicaid revenue in the first quarter of 2024, up from $6.3 billion in the same quarter a year earlier.
On April 26, Centene reported that its Medicaid enrollment fell 18.5% to 13.3 million in the first quarter of 2024 compared with the same period a year ago. The company's Medicaid revenue dipped 3% to $22.2 billion.
Unlike UnitedHealthcare, whose Medicaid enrollment fell to 7.7 million in March 2024 from 8.4 million a year prior, Molina's Medicaid enrollment rose in the first quarter of 2024 to 5.1 million from 4.8 million in March 2023. Molina's enrollment jump last year was partly a result of its having bought a Medicaid plan in Wisconsin and gained a new Medicaid contract in Iowa, the company said in its earnings news release.
Molina added 1 million members because states were prohibited from terminating Medicaid coverage during the pandemic. The company has lost 550,000 of those people during the unwinding and expects to lose an additional 50,000 by June.
About 90% of Molina Medicaid members have gone through the redetermination process, Zubretsky said.
The corporate giants also offset the enrollment losses by getting more Medicaid money from states, which they use to pass on higher payments to certain facilities or providers, Schneider said. By holding the money temporarily, the companies can count these “directed payments” as revenue.
Medicaid health plans were big winners during the pandemic after the federal government prohibited states from dropping people from the program, leading to a surge in enrollment to about 93 million Americans.
States made efforts to limit health plans' profits by clawing back some payments above certain thresholds, said Elizabeth Hinton, an associate director at KFF.
But once the prohibition on dropping Medicaid enrollees was lifted last spring, the plans faced uncertainty. It was unclear how many people would lose coverage or when it would happen. Since the unwinding began, more than 20 million people have been dropped from the rolls.
Medicaid enrollees' health care costs were lower during the pandemic, and some states decided to exclude pandemic-era cost data as they considered how to set payment rates for 2024. That provided yet another win for the Medicaid health plans.
Most states are expected to complete their Medicaid unwinding processes this year.
——————————
By: Phil Galewitz, KFF Health News
Title: Millions Were Booted From Medicaid. The Insurers That Run It Gained Medicaid Revenue Anyway.
Sourced From: kffhealthnews.org/news/article/medicaid-unwinding-insurer-revenue/
Published Date: Fri, 26 Apr 2024 13:55:00 +0000
Did you miss our previous article…
https://www.biloxinewsevents.com/california-is-investing-500m-in-therapy-apps-for-youth-advocates-fear-it-wont-pay-off/
Kaiser Health News
California Is Investing $500M in Therapy Apps for Youth. Advocates Fear It Won’t Pay Off.
Molly Castle Work
Fri, 26 Apr 2024 09:00:00 +0000
With little pomp, California launched two apps at the start of the year offering free behavioral health services to youths to help them cope with everything from living with anxiety to body acceptance.
Through their phones, young people and some caregivers can meet BrightLife Kids and Soluna coaches, some who specialize in peer support or substance use disorders, for roughly 30-minute virtual counseling sessions that are best suited to those with more mild needs, typically those without a clinical diagnosis. The apps also feature self-directed activities, such as white noise sessions, guided breathing, and videos of ocean waves to help users relax.
“We believe they're going to have not just great impact, but wide impact across California, especially in places where maybe it's not so easy to find an in-person behavioral health visit or the kind of coaching and supports that parents and young people need,” said Gov. Gavin Newsom's health secretary, Mark Ghaly, during the Jan. 16 announcement.
The apps represent one of the Democratic governor's major forays into health technology and come with four-year contracts valued at $498 million. California is believed to be the first state to offer a mental health app with free coaching to all young residents, according to the Department of Health Care Services, which operates the program.
However, the rollout has been slow. So slow that one of the companies has missed a deadline to make its app available on Android phones. Only about 15,000 of the state's 12.6 million children and young adults have signed up for the apps, and school counselors say they've never heard of them.
Advocates for youth question the wisdom of investing taxpayer dollars in two private companies. Social workers are concerned the companies' coaches won't properly identify youths who need referrals for clinical care. And the spending is drawing lawmaker scrutiny amid a state deficit pegged at as much as $73 billion.
An App for That
Newsom's administration says the apps fill a need for young Californians and their families to access professional telehealth for free, in multiple languages, and outside of standard 9-to-5 hours. It's part of Newsom's sweeping $4.7 billion master plan for kids' mental health, which was introduced in 2022 to increase access to mental health and substance use support services. In addition to launching virtual tools such as the teletherapy apps, the initiative is working to expand workforce capacity, especially in underserved areas.
“The reality is that we are rarely 6 feet away from our devices,” said Sohil Sud, director of Newsom's Children and Youth Behavioral Health Initiative. “The question is how we can leverage technology as a resource for all California youth and families, not in place of, but in addition to, other behavioral health services that are being developed and expanded.”
The virtual platforms come amid rising depression and suicide rates among youth and a shortage of mental health providers. Nearly half of California youths from the ages of 12 to 17 report having recently struggled with mental health issues, with nearly a third experiencing serious psychological distress, according to a 2021 study by the UCLA Center for Health Policy Research. These rates are even higher for multiracial youths and those from low-income families.
But those supporting youth mental health at the local level question whether the apps will move the needle on climbing depression and suicide rates.
“It's fair to applaud the state of California for aggressively seeking new tools,” said Alex Briscoe of California Children's Trust, a statewide initiative that, along with more than 100 local partners, works to improve the social and emotional health of children. “We just don't see it as fundamental. And we don't believe the youth mental health crisis will be solved by technology projects built by a professional class who don't share the lived experience of marginalized communities.”
The apps, BrightLife Kids and Soluna, are operated by two companies: Brightline, a 5-year-old venture capital-backed startup; and Kooth, a London-based publicly traded company that has experience in the U.K. and has also signed on some schools in Kentucky and Pennsylvania and a health plan in Illinois. In the first five months of Kooth's Pennsylvania pilot, 6% of students who had access to the app signed up.
Brightline and Kooth represent a growing number of health tech firms seeking to profit in this space. They beat out dozens of other bidders including international consulting companies and other youth telehealth platforms that had already snapped up contracts in California.
Although the service is intended to be free with no insurance requirement, Brightline's app, BrightLife Kids, is folded into and only accessible through the company's main app, which asks for insurance information and directs users to paid licensed counseling options alongside the free coaching. After KFF Health News questioned why the free coaching was advertised below paid options, Brightline reordered the page so that, even if a child has high-acuity needs, free coaching shows up first.
The apps take an expansive view of behavioral health, making the tools available to all California youth under age 26 as well as caregivers of babies, toddlers, and children 12 and under. When KFF Health News asked to speak with an app user, Brightline connected a reporter with a mother whose 3-year-old daughter was learning to sleep on her own.
‘It's Like Crickets'
Despite being months into the launch and having millions in marketing funds, the companies don't have a definitive rollout timeline. Brightline said it hopes to have deployed teams across the state to present the tools in person by midyear. Kooth said developing a strategy to hit every school would be “the main focus for this calendar year.”
“It's a big state — 58 counties,” Bob McCullough of Kooth said. “It'll take us a while to get to all of them.”
Brightline's contract states that the company was required to launch downloadable apps for iOS and Android phones by January, but so far BrightLife Kids is available only on Apple phones. Brightline said it's aiming to launch the Android version over the summer.
“Nobody's really done anything like this at this magnitude, I think, in the U.S. before,” said Naomi Allen, a co-founder and the CEO of Brightline. “We're very much in the early innings. We're already learning a lot.”
The contracts, obtained by KFF Health News through a records request, show the companies operating the two apps could earn as much as $498 million through the contract term, which ends in June 2027, months after Newsom is set to leave office. And the state is spending hundreds of millions more on Newsom's virtual behavioral health strategy. The state said it aims to make the apps available long-term, depending on usage.
The state said 15,000 people signed up in the first three months. When KFF Health News asked how many of those users actively engaged with the app, it declined to say, noting that data would be released this summer.
KFF Health News reached out to nearly a dozen California mental health professionals and youths. None of them were aware of the apps.
“I'm not hearing anything,” said Loretta Whitson, executive director of the California Association of School Counselors. “It's like crickets.”
Whitson said she doesn't think the apps are on “anyone's” radar in schools, and she doesn't know of any schools that are actively advertising them. Brightline will be presenting its tool to the counselor association in May, but Whitson said the company didn't reach out to plan the meeting; she did.
Concern Over Referrals
Whitson isn't comfortable promoting the apps just yet. Although both companies said they have a clinical team on staff to assist, Whitson said she's concerned that the coaches, who aren't all licensed therapists, won't have the training to detect when users need more help and refer them to clinical care.
This sentiment was echoed by other school-based social workers, who also noted the apps' duplicative nature — in some counties, like Los Angeles, youths can access free virtual counseling sessions through Hazel Health, a for-profit company. Nonprofits, too, have entered this space. For example, Teen Line, a peer-to-peer hotline operated by Southern California-based Didi Hirsch Mental Health Services, is free nationwide.
While the state is also funneling money to the schools as part of Newsom's master plan, students and school-based mental health professionals voiced confusion at the large app investment when, in many school districts, few in-person counseling roles exist, and in some cases are dwindling.
Kelly Merchant, a student at College of the Desert in Palm Desert, noted that it can be hard to access in-person therapy at her school. She believes the community college, which has about 15,000 students, has only one full-time counselor and one part-time bilingual counselor. She and several students interviewed by KFF Health News said they appreciated having engaging content on their phone and the ability to speak to a coach, but all said they'd prefer in-person therapy.
“There are a lot of people who are seeking therapy, and people close to me that I know. But their insurances are taking forever, and they're on the waitlist,” Merchant said. “And, like, you're seeing all these people struggle.”
Fiscal conservatives question whether the money could be spent more effectively, like to bolster county efforts and existing youth behavioral health programs.
Republican state Sen. Roger Niello, vice chair of the Senate Budget and Fiscal Review Committee, noted that California is forecasted to face deficits for the next three years, and taxpayer watchdogs worry the apps might cost even more in the long run.
“What starts as a small financial commitment can become uncontrollable expenses down the road,” said Susan Shelley of the Howard Jarvis Taxpayers Association.
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
——————————
By: Molly Castle Work
Title: California Is Investing $500M in Therapy Apps for Youth. Advocates Fear It Won't Pay Off.
Sourced From: kffhealthnews.org/news/article/california-youth-teletherapy-apps-rollout-slow/
Published Date: Fri, 26 Apr 2024 09:00:00 +0000
-
Local News4 days ago
Sister of Mississippi man who died after police pulled him from car rejects lawsuit settlement
-
Mississippi Today4 days ago
At Lake High School in Scott County, the Un-Team will never be forgotten
-
Mississippi Today24 hours ago
On this day in 1951
-
Mississippi News2 days ago
One injured in Mississippi officer-involved shooting after chase
-
Mississippi News7 days ago
Cicadas expected to takeover north Mississippi counties soon
-
Mississippi News6 days ago
Viewers make allegations against Hatley teacher, school district releases statement – Home – WCBI TV
-
Mississippi News Video5 days ago
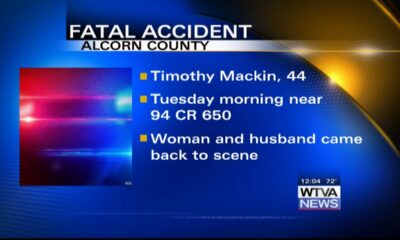
Vehicle struck and killed man lying in the road, Alcorn County sheriff says
-
Mississippi Today7 days ago
On this day in 1892