AP Photo/Elise Amendola
Jason P. Joseph, University of Florida
Former President Joe Biden has been diagnosed with an “aggressive” form of prostate cancer that has spread to his bones. But what does it mean for this type of cancer to be called aggressive?
As a urologic surgeon who specializes in diagnosing and treating prostate cancer, I often explain to my patients that aggressiveness isn’t based on a single factor. Instead, it comes from understanding how abnormal the cancer cells look, known as the tumor’s grade; how far they’ve spread, known as the tumor’s stage; and their genetic fingerprint.
Grade: Decoding cancer cell appearance
One key piece of the puzzle is the cancer’s grade, which indicates the tumor’s potential to grow. After a prostate biopsy, a doctor specializing in examining tissues – a pathologist – grades the tumor by comparing the appearance of its cancer cells with that of normal prostate cells.
Imagine healthy prostate cells as organized workers in a factory, each performing specific tasks. In contrast, high-grade cancer cells appear chaotic, growing and dividing rapidly.
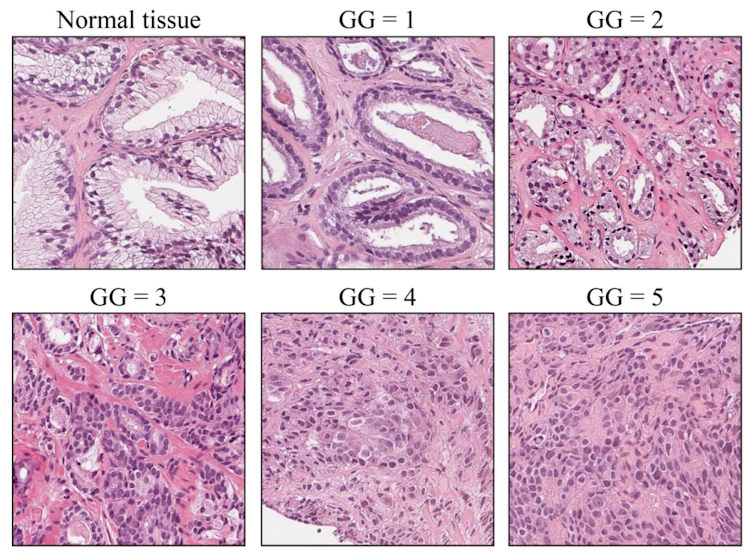
Salvi et al/Cancers, CC BY-SA
For prostate cancer, doctors use what are called grade groups that range from 1 (least aggressive) to 5 (most aggressive). These groups are a simplification based on an older classification called a Gleason score. Biden’s Gleason 9 cancer falls into grade group 5, indicating the cells appear extremely abnormal with a strong potential for rapid growth and spread.
While the cancer’s grade helps indicate how tumor cells might behave, it doesn’t tell the whole story. Some high-grade cancers can remain confined to the prostate for months or even years.
To understand where the cancer is and how far it has advanced, doctors determine its stage.
Stage: Mapping cancer location and spread
A tumor’s stage describes if, and how far, cancer has spread beyond where it first formed. Doctors use physical exams, imaging scans and lab tests to stage prostate cancer.
Medical professionals usually use a detailed system called TNM – short for tumor, nodes, metastasis – to classify a tumor’s stage. But prostate cancer stage can be broadly understood as:
-
Localized (stages 1-2): The cancer is only within the prostate. Think of a weed confined to a small garden bed. Many localized cancers, particularly if low-grade, may not be deemed aggressive and can often be safely monitored.
-
Locally advanced (Stage 3): The cancer has spread out from the prostate and is growing in very nearby tissues, like a weed sending roots into the surrounding lawn.
-
Metastatic (Stage 4): The cancer has spread to distant parts of the body. For prostate cancer, this often means lymph nodes, bones – as in Biden’s case – liver or lungs. This is like the weeds spreading seeds down the street and across town.
A Stage 4 prostate cancer is considered advanced and aggressive because it has shown that it can travel and form new tumors.
A tumor’s stage heavily influences treatment options and goals. For localized or some locally advanced cancers (Stage 1 to Stage 3), treatments such as surgery or radiation may aim for a cure. For metastatic cancer, a cure is usually not possible. Treatment focuses on controlling growth, managing symptoms and maintaining quality of life.
Many prostate cancers rely on hormones called androgens as fuel for their growth. Therapies that block these hormones can be effective for some time – in most cases, years – especially for hormone-sensitive cancers like Biden’s.
Fortunately, thanks to improved screening options and increased awareness, about 69% of prostate cancers are found when they are still confined to the prostate (Stage 1 to Stage 2). About 8% of new cases are metastatic at diagnosis.
Genetics: Uncovering cancer’s DNA blueprint
In addition to grade and stage, doctors are increasingly using a cancer’s genomic profile – its specific genetic makeup – both for deeper insights into its aggressiveness and potential treatment pathways.
DNA acts like a detailed instruction manual for cells, dictating how they should grow and function as well as when they should stop dividing or die. In cancer, mutations act like typos in this genetic instruction manual, causing cells to ignore these normal controls, grow and spread.
Genomic testing can identify these specific genetic alterations. This can be performed on the tumor tissue itself to identify changes called somatic mutations that occurred after you were born. Or it can be carried out through blood or saliva samples to detect changes you inherited called germline mutations.
For men with early-stage prostate cancer, certain genomic tests on the tumor can help clarify the risk of the cancer progressing. This information is valuable in deciding whether active surveillance – closely monitoring the cancer without immediate treatment – is a safe approach, or whether more immediate treatment is warranted.
In advanced or metastatic prostate cancer, identifying specific mutations is particularly critical. For instance, mutations in genes such as BRCA1 or BRCA2 – more commonly associated with breast and ovarian cancer risk – can also occur in prostate cancer. These mutations can make the cancer more aggressive but also potentially susceptible to a specific type of drug called a PARP inhibitor, especially if the cancer becomes resistant to hormone therapy.
National guidelines now recommend genomic testing for all men with metastatic prostate cancer to look for these “actionable” mutations. This move toward personalized medicine means treatments can be increasingly tailored to the unique fingerprint of a patient’s cancer.
Understanding cancer ‘aggressiveness’
It’s essential to understand that “aggressive” isn’t just a simple label for cancer, but rather a multilayered evaluation. An aggressive-looking cancer caught early and confined to the prostate (Stage 1 and Stage 2) can have a nearly 100% five-year relative survival rate. However, if the same high-grade cancer has already spread widely (Stage 4), five-year relative survival drops significantly, to around 38%.
This stark difference in survival rates highlights a critical point. To obtain the clearest picture of a cancer’s potential threat, a comprehensive assessment combines insights from multiple qualities of a tumor to help patients and their health care teams make informed decisions.
Thankfully, advances in genomics, imaging and targeted therapies continue to improve how aggressiveness is defined, how its behavior is predicted and how treatment is personalized. This progress offers growing hope for better outcomes, even for patients with the most aggressive prostate cancers.
Jason P. Joseph, Assistant Professor of Urology, University of Florida
This article is republished from The Conversation under a Creative Commons license. Read the original article.