Tetra Images via Getty Images
Julio Fernandez-Mendoza, Penn State
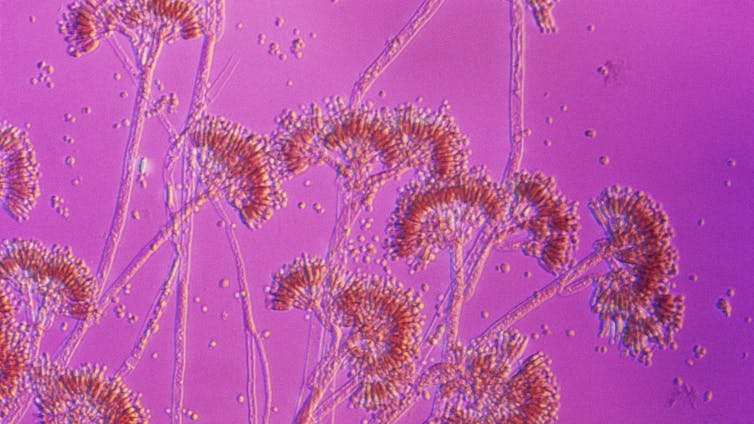
About 10% of Americans say they have chronic insomnia, and millions of others report poor sleep quality. Ongoing research has found that bad sleep could lead to numerous health problems, including heart disease.
Dr. Julio Fernandez-Mendoza is a professor of psychiatry and behavioral health, neuroscience and public health sciences at Penn State College of Medicine. He discusses the need for sleep, why teenagers require more sleep than adults, and how you can get a good night’s sleep without medications.
The Conversation has collaborated with SciLine to bring you highlights from the discussion that have been edited for brevity and clarity.
How much sleep is enough for adults and for adolescents?
Julio Fernandez-Mendoza: Adults who report getting about seven to eight hours of sleep per night generally have the best health, in terms of both physical and mental health, and longevity.
But that recommendation changes with age. Adults over age 65 may need just six to seven hours of sleep per night. So older people, if otherwise healthy, should not feel anxious if they’re getting just six hours. Young people need the most – at least nine hours – and some younger children may need more.
How can insufficient sleep harm our health?
Fernandez-Mendoza: Our team was the first to show that those complaining about insomnia – difficulty falling or staying asleep – were more likely to have high blood pressure and be at risk for heart disease.
In both teens and adults, we found that insomnia and shortened sleep may lead to elevated stress, hormone levels and inflammation. These problems tend to show up before you develop heart disease.
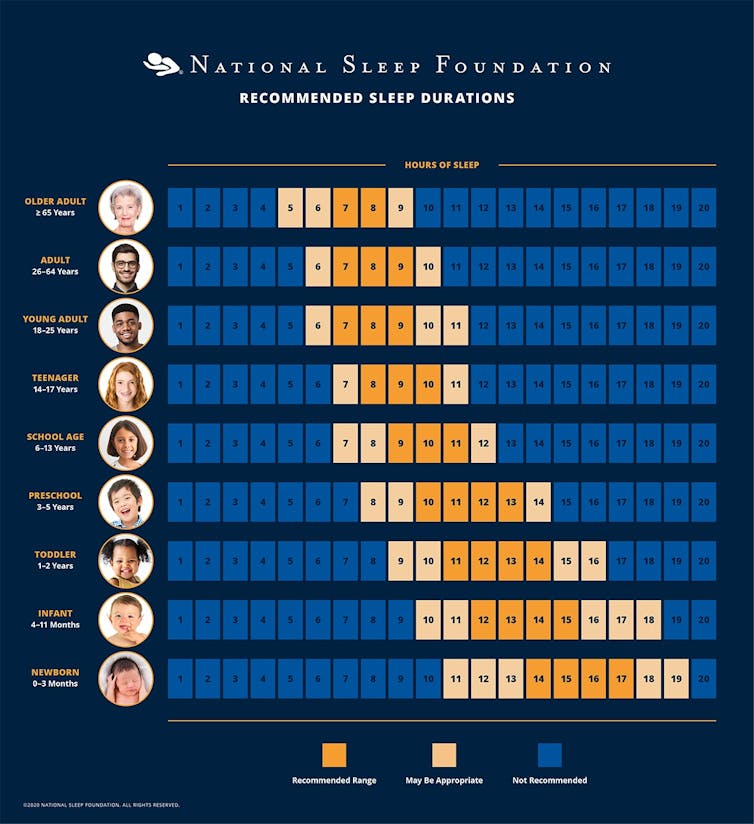
National Sleep Foundation Copyright 2025 National Sleep Foundation, all rights reserved
What about people who have more serious sleep problems?
Fernandez-Mendoza: Good sleep hygiene habits include cutting down on caffeine and alcohol, quitting smoking and exercising regularly. I also recommend not skipping meals, not eating too late at night and not eating too much.
But people with a persistent sleep problem may need to make more behavioral changes. Research studies point to a set of six rules that can improve your sleep. You can follow these changes consistently in the short term, and then choose how to adapt them into your lifestyle down the road.
First, get up at the same time no matter what. No matter how much sleep you get. This will anchor your sleep/wake cycle, called your circadian rhythm.
Second, do not use your bed for anything except sleep and sexual activity.
Third, when you can’t sleep, don’t lie in bed awake. Instead, get out of bed, go into another room if you can, and do an activity that’s enjoyable or relaxing. Go back to bed only when you’re ready to sleep.
Fourth, get going with daily activities even after a poor night’s sleep. Don’t try to compensate for sleep loss. If you have chronic insomnia, don’t nap, sleep in, or doze during the day or evening even after poor sleep the previous night.
Fifth, go to bed only when you’re actually sleepy enough to fall asleep.
And sixth, start with the amount of sleep you’re now getting – with the lowest limit at five hours – and then increase it weekly by 15 minutes.
These six rules are evidence-based and go above and beyond simple sleep hygiene habits. If they don’t work, see a provider who can help you.
Do you have advice specifically for adolescents?
Fernandez-Mendoza: Adolescence is a unique developmental period. It’s not just the obvious physical, emotional and behavioral changes that occur during adolescence and puberty – there are changes in a teenager’s brain that can alter their sleep patterns.
When an adolescent goes through puberty, their internal clock changes so that their sleep schedule shifts to later hours. While it’s true that adolescents are more engaged at night because of their social relationships, there’s also biology behind why they want to stay up late – their internal clocks have shifted. It’s not just choice.
School start times for most adolescents are at odds with that biological shift. So they don’t get enough sleep, which affects their performance in school. Research suggests that schools with later start times are more closely aligned with the science on child development and don’t put adolescents at risk by making them wake up earlier than their bodies are biologically inclined to.
Parents can help their teens get better sleep. Set a time for kids to stop doing homework and put away electronics. Instead, they can watch TV with the family or read – something relaxing and enjoyable that will help them wind down before bed.
You can also gradually move back their wake-up time. Start on weekends, waking them up 30 minutes earlier every day, including school days, until the child reaches the desired wake-up time. Don’t try to reshift them suddenly – for example, waking up a teenager at 5 a.m. like it’s the military – because that doesn’t work. They won’t get used to it, since it’s at odds with their internal clock. So, do it little by little. If that doesn’t work, see a clinical provider.
What kind of treatments can a sleep clinician provide?
Fernandez-Mendoza: People should get help if they feel they sleep poorly, if they’re fatigued during the day, or if they snore or grind their teeth. All these issues deserve attention.
Some people may think a sleep provider just prescribes expensive medication, but that’s not true. There are behavioral, non-drug-based treatments that work. Cognitive behavioral therapy is the first-line treatment recommended for insomnia. Light therapy may also help, which is the use of a bright light therapy lamp at a given time during the day or evening, depending on the person’s sleep problem.
Watch the full interview to hear more.
SciLine is a free service based at the American Association for the Advancement of Science, a nonprofit that helps journalists include scientific evidence and experts in their news stories.
Julio Fernandez-Mendoza, Professor of Psychiatry and Behavioral Health, Neuroscience, and Public Health Sciences, Penn State
This article is republished from The Conversation under a Creative Commons license. Read the original article.