Digicomphoto/ Science Photo Library via Getty Images
Hanna D. Paton, University of Iowa
The flu sickens millions of people in the U.S. every year, and the past year has been particularly tough. Although infections are trending downward, the Centers for Disease Control and Prevention has called the winter of 2024-2025 a “high severity” season with the highest hospitalization rate in 15 years.
Since early 2024, a different kind of flu called bird flu, formally known as avian influenza, has been spreading in birds as well as in cattle. The current bird flu outbreak has infected 70 Americans and caused two deaths as of April 8, 2025. Public health and infectious disease experts say the risk to people is currently low, but they have expressed concern that this strain of the bird flu virus may mutate to spread between people.
As a doctoral candidate in immunology, I study how pathogens that make us sick interact with our immune system. The viruses that cause seasonal flu and bird flu are distinct but still closely related. Understanding their similarities and differences can help people protect themselves and their loved ones.
What is influenza?
The flu has long been a threat to public health. The first recorded influenza pandemic occurred in 1518, but references to illnesses possibly caused by influenza stretch back as as early as 412 B.C., to a treatise called Of the Epidemics by the Greek physician Hippocrates.
Today, the World Health Organization estimates that the flu infects 1 billion people every year. Of these, 3 million to 5 million infections cause severe illness, and hundreds of thousands are fatal.
Influenza is part of a large family of viruses called orthomyxoviruses. This family contains several subtypes of influenza, referred to as A, B, C and D, which differ in their genetic makeup and in the types of infections they cause. Influenza A and B pose the largest threat to humans and can cause severe disease. Influenza C causes mild disease, and influenza D is not known to infect people. Since the turn of the 20th century, influenza A has caused four pandemics. Influenza B has never caused a pandemic.
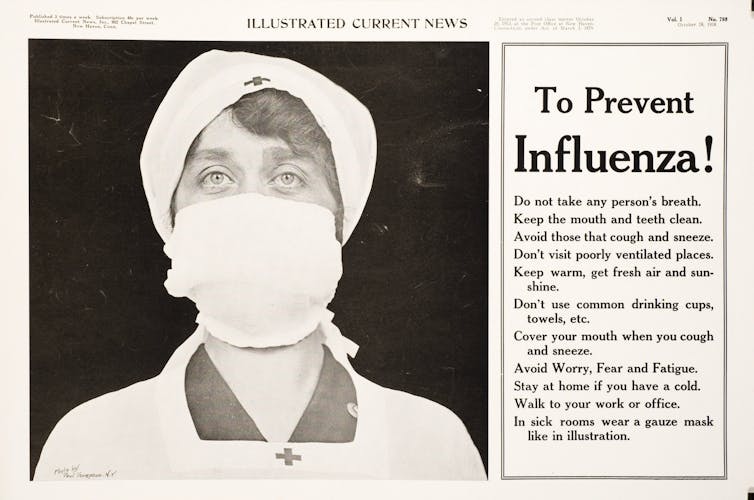
Illustrated Current News/National Library of Medicine, CC BY
An influenza A strain called H1N1 caused the famous 1918 Spanish flu pandemic, which killed about 50 million people worldwide. A related H1N1 virus was responsible for the most recent influenza A pandemic in 2009, commonly referred to as the swine flu pandemic. In that case, scientists believe multiple different types of influenza A virus mixed their genetic information to produce a new and especially virulent strain of the virus that infected more than 60 million people in the U.S. from April 12, 2009, to April 10, 2010, and caused huge losses to the agriculture and travel industries.
Both swine and avian influenza are strains of influenza A. Just as swine flu strains tend to infect pigs, avian flu strains tend to infect birds. But the potential for influenza A viruses that typically infect animals to cause pandemics in humans like the swine flu pandemic is why experts are concerned about the current avian influenza outbreak.
Seasonal flu versus bird flu
Different strains of influenza A and influenza B emerge each year from about October to May as seasonal flu. The CDC collects and analyzes data from public health and clinical labs to determine which strains are circulating through the population and in what proportions. For example, recent data shows that H1N1 and H3N2, both influenza A viruses, were responsible for the vast majority of cases this season. Standard tests for influenza generally determine whether illness is caused by an A or B strain, but not which strain specifically.
Officials at the Food and Drug Administration use this information to make strain recommendations for the following season’s influenza vaccine. Although the meeting at which FDA advisers were to decide the makeup of the 2026 flu vaccine was unexpectedly canceled in late February, the FDA still released its strain recommendations to manufacturers.
The recommendations do not include H5N1, the influenza A strain that causes avian flu. The number of strains that can be added into seasonal influenza vaccines is limited. Because cases of people infected with H5N1 are minimal, population-level vaccination is not currently necessary. As such, seasonal flu vaccines are not designed to protect against avian influenza. No commercially available human vaccines currently exist for avian influenza viruses.
How do people get bird flu?
Although H5N1 mainly infects birds, it occasionally infects people, too. Human cases, first reported in 1997 in Hong Kong, have primarily occurred in poultry farm workers or others who have interacted closely with infected birds.
Initially identified in China in 1996, the first major outbreak of H5 family avian flu occurred in North America in 2014-2015. This 2014 outbreak was caused by the H5N8 strain, a close relative of H5N1. The first H5N1 outbreak in North America began in 2021 when infected birds carried the virus across the ocean. It then ripped through poultry farms across the continent.

NIAID and CDC/flickr, CC BY
In March 2024, epidemiologists identified H5N1 infections in cows on dairy farms. This is the first time that bird flu was reported to infect cows. Then, on April 1, 2024, health officials in Texas reported the first case of a person catching bird flu from infected cattle. This was the first time transmission of bird flu between mammals was documented.
As of March 21, 2025, there have been 988 human cases of H5N1 worldwide since 1997, about half of which resulted in death. The current outbreak in the U.S. accounts for 70 of those infections and one death. Importantly, there have been no reports of H5N1 spreading directly from one person to another.
Since avian flu is an influenza A strain, it would show up as positive on a standard rapid flu test. However, there is no evidence so far that avian flu is significantly contributing to current influenza cases. Specific testing is required to confirm that a person has avian flu. This testing is not done unless there is reason to believe the person was exposed to sick birds or other sources of infection.
How might avian flu become more dangerous?
As viruses replicate within the cells of their host, their genetic information can get copied incorrectly. Some of these genetic mutations cause no immediate differences, while others alter some key viral characteristics.
Influenza viruses mutate in a special way called reassortment, which occurs when multiple strains infect the same cell and trade pieces of their genome with one another, potentially creating new, unique strains. This process prolongs the time the virus can inhabit a host before an infection is cleared. Even a slight change in a strain of influenza can result in the immune system’s inability to recognize the virus. As a result, this process forces our immune systems to build new defenses instead of using immunity from previous infections.
Reassortment can also change how harmful strains are to their host and can even enable a strain to infect a different species of host. For example, strains that typically infect pigs or birds may acquire the ability to infect people. Influenza A can infect many different types of animals, including cattle, birds, pigs and horses. This means there are many strains that can intermingle to create novel strains that people’s immune systems have not encountered before – and are therefore not primed to fight.
It is possible for this type of transformation to also occur in H5N1. The CDC monitors which strains of flu are circulating in order prepare for that possibility. Additionally, the U.S. Department of Agriculture has a surveillance system for monitoring potential threats for spillover from birds and other animals, although this capacity may be at risk due to staff cuts in the department.
These systems are critical to ensure that public health officials have the most up-to-date information on the threat that H5N1 poses to public health and can take action as early as possible when a threat is evident.
Hanna D. Paton, PhD Candidate in Immunology, University of Iowa
This article is republished from The Conversation under a Creative Commons license. Read the original article.