Viktoriya Skorikova/Moment via Getty Images
Cynthia H. Chuang, Penn State and Carol S. Weisman, Penn State
On June 24, 2022, the U.S. Supreme Court decision in Dobbs v. Jackson Women’s Health Organization eliminated a nearly 50-year constitutional right to abortion and returned the authority to regulate abortion to the states.
The Dobbs ruling, which overturned Roe v. Wade, has vastly reshaped the national abortion landscape. Three years on, many states have severely restricted access to abortion care. But the decision has also had a less well-recognized outcome: It is increasingly jeopardizing access to contraception.
We are a physician scientist and a sociologist and health services researcher studying women’s health care and policy, including access to contraception. We see a worrisome situation emerging.
Even while the growing limits on abortion in the U.S. heighten the need for effective contraception, family planning providers are less available in many states, and health insurance coverage of some of the most effective types of contraception is at risk.
A growing demand for contraception
Abortion restrictions have proliferated around the country since the Dobbs decision. As of June 2025, 12 states have near-total abortion bans and 10 states ban abortion before 23 or 24 weeks of gestation, which is when a fetus is generally deemed viable. Of the remaining states, 19 restrict abortion after viability and nine states and Washington have no gestational limits.
It’s no surprise that women living in states that ban or severely restrict abortion may be especially motivated to avoid unintended pregnancy. Even planned pregnancies have grown riskier, with health care providers fearing legal repercussions for treating pregnancy-related medical emergencies such as miscarriages. Such concerns may in part explain emerging research that suggests the use of long-acting contraception such as intrauterine devices, or IUDs, and permanent contraception – namely, sterilization – are on the rise.
A national survey conducted in 2024 asked women ages 18 to 49 if they have changed their contraception practices “as a result of the Supreme Court overturning Roe v. Wade.” It found that close to 1 in 5 women began using contraception for the first time, switched to a more effective contraceptive method, received a sterilization procedure or purchased emergency contraception to keep on hand.
A study in Ohio hospitals found a nearly 16% increase in women choosing long-acting contraception methods or sterilization in the six months after the Dobbs decision, and a 33% jump in men receiving vasectomies. Another study, which looked at both female and male sterilization in academic medical centers across the country, also reported an uptick in sterilization procedures for young adults ages 18 to 30 after the Dobbs decision, through 2023.
A loss of contraception providers
Ironically, banning or severely restricting abortion statewide may also diminish capacity to provide contraception.
To date, there is no compelling evidence that OB-GYN doctors are leaving states with strict abortion laws in significant numbers. One study found that states with severe abortion restrictions saw a 4.2% decrease in such practitioners compared with states without abortion restrictions.
However, the Association of American Medical Colleges reports declining applications to residency training programs located in states that have abortion bans – not just for OB-GYN training programs, but for residency training of all specialties. This drop suggests that doctors may be overall less likely to train in states that restrict medical practice. And given that physicians often stay on to practice in the states where they do their training, it may point to a long-term decline in physicians in those states.
But the most significant drop in contraceptive services likely comes from the closure of abortion clinics in states with the most restrictive abortion policies. That’s because such clinics generally provide a wide range of reproductive services, including contraception. The 12 states with near-total abortion bans had 57 abortion clinics in 2020, all of which were closed as of March 2024. One study reported a 4.1% decline in oral contraceptives dispensed in those states.
Contraception under threat
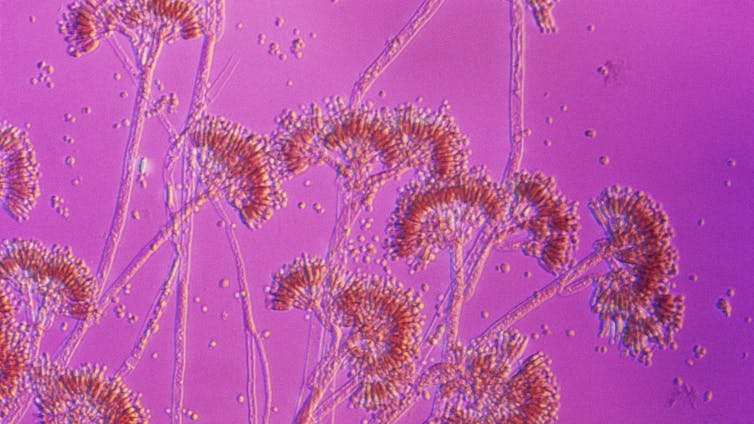
The Dobbs decision has also encouraged ongoing efforts to incorrectly redefine some of the most effective contraceptives as medications that cause abortion. These efforts target emergency contraceptive pills, known as Plan B over-the-counter and Ella by prescription, as well as certain IUDs. Emergency contraceptive pills are up to 98% effective at preventing pregnancy after unprotected sex, and IUDs are 99% effective.
Neither method terminates a pregnancy, which by definition begins when a fertilized egg implants in the uterus. Instead, emergency contraceptive pills prevent an egg from being released from the ovaries, while IUDs, depending on the type, prevent sperm from fertilizing an egg or prevent an egg from implanting in the uterus.
Conflating contraception and abortion spreads misinformation and causes confusion. People who believe that certain types of contraception cause abortions may be dissuaded from using those methods and rely on less effective methods. What’s more, it may affect health insurance coverage.
Medicaid, which provides health insurance for low-income children and adults, has been required to cover family planning services at no cost to patients since 1972. Since 2012, the Affordable Care Act has required private health insurers to cover certain women’s health preventive services at no cost to patients, including the full-range of contraceptives approved by the Food and Drug Administration.
According to our research, the insurance coverage required by the Affordable Care Act has increased use of IUDs, which can be prohibitively expensive when paid out of pocket. But if IUDs and emergency contraceptive pills were reclassified as interventions that induce abortion, they likely would not be covered by Medicaid or the Affordable Care Act, since neither type of health insurance requires coverage for abortion care. Thus, access to some of the most effective contraceptive methods could be jeopardized at a time when the right to terminate an unintended or nonviable pregnancy has been rolled back in much of the country.
Indeed, Project 2025, the conservative policy agenda that the Trump administration appears to be following, specifically calls for removing Ella from the Affordable Care Act contraception coverage mandate because it is a “potential abortifacient.” And politicians in multiple states have expressed support for the idea of restricting these contraceptive methods, as well as contraception more broadly.
On the third anniversary of the Dobbs decision, it is clear that its ripple effects include threats to contraception. Considering that contraception use is almost universal among women in their reproductive years, in our view these threats should be taken seriously.
Cynthia H. Chuang, Professor of Medicine and Public Health Sciences, Penn State and Carol S. Weisman, Distinguished Professor Emerita of Public Health Sciences, Penn State
This article is republished from The Conversation under a Creative Commons license. Read the original article.