News from the South - Alabama News Feed
States try to rein in health insurers’ claim denials, with mixed results
by Shalina Chatlani, Alabama Reflector
March 25, 2025
This story originally appeared on Stateline.
Health insurance companies are under increasing scrutiny for allegedly using artificial intelligence bots and algorithms to swiftly deny patients routine or lifesaving care — without a human actually reviewing their claims.
The high-profile killing late last year of UnitedHealthcare CEO Brian Thompson has focused even more attention on so-called prior authorization, the process by which patients and doctors must ask health insurers to approve medical procedures or drugs before proceeding. There had been protests and outrage over the company’s practices for months before Thompson’s death, and UnitedHealthcare has been accused in a class-action lawsuit of using AI to wrongfully deny claims.
As more patients and doctors voice their frustrations, states are responding with legislation designed to regulate prior authorization and claims reviews. So far this year, lawmakers in more than a dozen states are considering measures that would, for example, limit the use of AI in reviewing claims; exclude certain prescription medications from prior authorization rules; ensure that emergency mental health care is not delayed for more than 48 hours; and require that insurers’ review boards include licensed physicians, dentists or pharmacists with clinical experience.
GET THE MORNING HEADLINES.
Insurers have long required doctors to obtain their approval before they’ll pay for certain drugs, treatments and procedures. They argue it is necessary to rein in health care costs and limit unnecessary services. But many doctors and patients say the practice has gotten out of hand, causing delays and denials of care that are harming and even killing people.
In a survey last year by the American Medical Association, 93% of doctors said that insurers’ prior authorization practices delayed “necessary care” for their patients. Twenty-nine percent said such delays had led to a “serious adverse event,” such as hospitalization, permanent injury or death.
In 2023, insurers selling plans on the marketplaces created under the Affordable Care Act denied a combined average of 20% of all claims. Of the 73 million in-network claims they denied, only 1% were appealed, according to KFF, a health policy research group.
The federal role
Under the Biden administration, the Federal Trade Commission and the Department of Justice took a firmer hand against health care corporations alleged to be engaging in behavior resulting in limited and more expensive care for patients. The administration also approved rules requiring that beginning in 2026, Medicare and Medicaid plans create a streamlined electronic process for reviewing claims, making decisions more quickly and providing specific reasons for denying care.
But it’s difficult to hold insurers accountable, according to Timothy McBride, a health policy analyst and co-director of a program at the Institute for Public Health at Washington University in St. Louis.
“Each part of the health care industry — hospitals, pharmaceuticals, insurers — they all have a lot of concentrated power,” McBride said in a phone interview. “And unless somebody actually takes it on directly, it’s going to stay that way. I think the Biden administration tried to take it on, but didn’t make a lot of progress.”
It’s unclear whether the Trump administration and Congress will reverse course. During his confirmation hearing on March 14, Dr. Mehmet Oz, President Donald Trump’s pick to lead the Centers for Medicare & Medicaid Services, defended the use of artificial intelligence in reviewing claims.
“AI can be used for good or for evil, and it to a large extent depends on who’s using it and for what purpose,” Oz told members of the U.S. Senate Finance Committee. “I think AI could play a vital role in accelerating preauthorization.”
In the past, Trump has supported measures to help patients, such as increasing hospital price transparency and lowering prescription drug prices, McBride noted. But “Republicans and conservatives generally are anti-regulation,” he said. “My gut feeling would be that they back off on the Biden push on this.”
States have limited power to act on their own. They have authority only over state-regulated health plans, which include Medicaid, plans for state workers and policies residents purchase from the ACA marketplaces. About 90 million people are covered that way. State laws do not apply to the 156 million workers, retirees and dependents who get their coverage through employer-sponsored health plans, which are regulated through a federal law known as ERISA.
Furthermore, health insurance companies are large and have deep pockets, allowing them to easily absorb state fines.
But Kaye Pestaina, the director of the program on patient and consumer protection at KFF, said states have an important role to play.
“Much of the focus around prior authorization at the federal level has kind of originated from state protections, so I imagine there will be continual activity by state legislatures to come at the problem,” Pestaina told Stateline.
What states are doing
Pestaina said states are trying a number of solutions. For example, states such as Arizona, Michigan and Pennsylvania have given their insurance regulators more authority to directly access claims denial information, in order to overturn decisions or potentially enforce state rules. And these efforts have largely had bipartisan support.
There is a role for some oversight to make sure that things are covered. But right now, I think the system is out of balance.
– North Carolina Republican state Rep. Timothy Reeder
In Pennsylvania, Republican state Sen. Kristin Phillips-Hill pushed through bipartisan legislation in 2022 to streamline prior authorization practices for state-regulated health plans after hearing numerous complaints from patients and doctors.
The legislation created an Independent External Review organization that allows Pennsylvanians to submit an online form to request a review if their insurer denies a service or treatment. If the review organization decides the service should be covered, the insurer must do so. Before then, patients could turn only to a federal review process, which may have been more challenging to navigate and taken more time.
“Our reforms created clear rules, clear timelines for the prior authorization process, and it removed ambiguity or uncertainty from the system that at times, insurers could exploit and providers could be confused over,” Phillips-Hill told Stateline. “Prior to that reform, if you had a denial from your insurer, you had very little recourse.”
The program began in January 2024, and in its first year the Pennsylvania Insurance Department overturned half of 517 denials, which amounted to claims from 259 people.
Jonathan Greer, president and CEO of the Insurance Federation of Pennsylvania, said his trade group worked with lawmakers to come to an agreement on how to change the prior authorization process in a way that worked for insurers and patient advocates. Greer says he thinks Pennsylvania could be a model for other states.
“Prior authorization, I think unfairly, has been characterized as a reason to say ‘no’ by insurers,” Greer said. “The purpose of prior authorization is to make sure that you know the care that you get is consistent with the care that you need.”
In North Carolina, Republican state Rep. Timothy Reeder is hopeful that his prior authorization bill will make it across the finish line this year. Reeder’s bill would set tight deadlines on insurers’ claim decisions and require companies to have licensed practitioners on their claim review boards. Insurers would also have to publicize a list of services they require authorization for.
“I’m not saying that we need to get rid of it completely,” Reeder told Stateline. “There is a role for some oversight to make sure that things are covered. But right now, I think the system is out of balance.”
But some state laws have proven to be less effective than advertised.
In 2021, Texas enacted a first-of-its-kind law creating a “gold card” standard, under which physicians whose care recommendations are approved by insurers at least 90% of the time are exempt from the prior authorization process. But as of the end of 2023, only 3% of Texas physicians had earned gold card status, according to the Texas Medical Association.
That’s why the group is pushing legislation that would require insurers to report which preauthorization exemptions they granted and denied and how many claims went to independent review. Dr. Zeke Silva of the Texas Medical Association’s legislative council said it would be “in the same spirit” as what Pennsylvania has done.
“Our focus with the [Texas Medical Association] is our physicians being able to provide the best care possible. And we want that to be free of burden,” Silva told Stateline. “We want to minimize third parties coming in and inappropriately denying care that our physicians and our patients think is in their best interest.”
Stateline reporter Shalina Chatlani can be reached at schatlani@stateline.org.
Stateline is part of States Newsroom, a nonprofit news network supported by grants and a coalition of donors as a 501c(3) public charity. Stateline maintains editorial independence. Contact Editor Scott S. Greenberger for questions: info@stateline.org.
YOU MAKE OUR WORK POSSIBLE.
Alabama Reflector is part of States Newsroom, a nonprofit news network supported by grants and a coalition of donors as a 501c(3) public charity. Alabama Reflector maintains editorial independence. Contact Editor Brian Lyman for questions: info@alabamareflector.com.
The post States try to rein in health insurers’ claim denials, with mixed results appeared first on alabamareflector.com
News from the South - Alabama News Feed
A very dry September forecast with hot afternoons ahead for Alabama.
SUMMARY: Alabama faces a very dry September with hot afternoons continuing through the last week of summer before the autumnal equinox. Sunday begins comfortably cool in the 60s, warming to low 90s by mid-afternoon under mostly sunny skies. A weak wave may bring a few showers tonight, mainly to northwest Alabama, but widespread rain is unlikely. Temperatures will remain above average, hitting mid-90s Tuesday and Wednesday. By next weekend, a trough and front may increase cloud cover and rain chances slightly, potentially lowering temperatures closer to average. Overall, the forecast calls for persistent dry and warm conditions into next week.
A very dry September forecast with hot afternoons ahead for Alabama.
WVTM13 is your home for Alabama breaking news and weather. For your latest Alabama news and weather visit: https://www.wvtm13.com/
For licensing inquiries: https://www.wvtm13.com/licensing
News from the South - Alabama News Feed
Huntsville Fire & Rescue Holds 9/11 Memorial Service | Sept. 11, 2025 | News 19 at 5 p.m.
SUMMARY: On September 11, 2025, Huntsville Fire & Rescue held a memorial service to honor the nearly 3,000 lives lost in the 9/11 terrorist attacks. Military members and first responders gathered at Huntsville Fire Station One, where at 7:46 a.m., lights, sirens, and air horns sounded to replicate the sounds heard during the attacks. Fire Chief Howard McFarland emphasized the importance of remembering the tragedy to educate younger generations and prevent history from repeating. Former Captain Lynn recalled the shock of witnessing the attacks and noted how 9/11 reshaped emergency preparedness. This annual event is held across all 20 Huntsville fire stations.
The Huntsville Fire & Rescue held a 9/11 memorial service.
News 19 is North Alabama’s News Leader! We are the CBS affiliate in North Alabama and the Tennessee Valley since November 28, 1963.
https://whnt.com/
https://www.facebook.com/whntnews19
https://www.instagram.com/whntnews19/
https://twitter.com/whnt
News from the South - Alabama News Feed
News 5 NOW at 8:00am | September 11, 2025
SUMMARY: On September 11, 2025, News 5 NOW covered 9/11 commemorations, including first responders climbing 2,000 steps at Hancock Whitney Stadium to honor the World Trade Center’s 110 stories. The Original Oyster House offered free meals to first responders in Mobile and Baldwin counties. The program also reported a new Vibrio bacterial infection case in Escambia County, highlighting health warnings for beachgoers. Additionally, they discussed a study linking chronic insomnia to increased dementia risk, election recounts in Gulf Shores, and a recent political shooting in Utah, sparking debate over harsher punishments for political violence. Viewer opinions on extraterrestrials and political violence were shared in an interactive social media segment.
First Responders in Mobile honored the heroes of September 11th, a Pensacola woman is in the hospital after being infected with the flesh eating bacteria vibrio vulnificus, and a vote re-count wrapped up in Gulf Shores…
-
News from the South - Kentucky News Feed7 days ago
Lexington man accused of carjacking, firing gun during police chase faces federal firearm charge
-
News from the South - Alabama News Feed7 days ago
Zaxby's Player of the Week: Dylan Jackson, Vigor WR
-
News from the South - Arkansas News Feed7 days ago
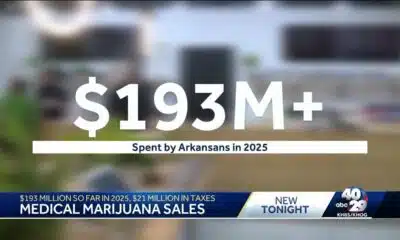
Arkansas medical marijuana sales on pace for record year
-
News from the South - North Carolina News Feed5 days ago
What we know about Charlie Kirk shooting suspect, how he was caught
-
Local News7 days ago
US stocks inch to more records as inflation slows and Oracle soars
-
Local News6 days ago
Russian drone incursion in Poland prompts NATO leaders to take stock of bigger threats
-
News from the South - North Carolina News Feed5 days ago
Federal hate crime charge sought in Charlotte stabbing | North Carolina
-
Local News Video6 days ago
Introducing our WXXV Student Athlete of the Week, St. Patrick’s Parker Talley!