Much of the small intestine microbiome remains an undiscovered frontier.
Christopher Damman, University of Washington
Microbiome research to date has been much like the parable of the blind men and the elephant. How much can be said about an elephant by examining just its tail? Researchers have studied what is most readily available – stool rescued from a flush down the toilet – but have been missing the microbial masterminds upstream in the small intestine. Until recently.
Likened by some scientists to another human organ, your microbiome is collectively the tens of trillions of microorganisms that live in interconnected populations on and in your body. They serve as miniature sentinels that help protect your body’s surfaces from pathogenic invaders. In the upper intestine, distinct microbial populations also aid in digestion, metabolism and even immunity.
I am a gastroenterologist who has spent the past 20 years studying the microbiome’s role in health and disease. Advances in technology are helping scientists investigate the small intestine microbiome and the promise it holds for better understanding and treating many diseases.
Big transformations come from small places
Certain members of the small intestine microbiome are linked to obesity and overweight, while other microbial members are linked to a healthy metabolic state. Indeed, small intestine microbes aid in digestion by turning certain simple carbohydrates into the molecular building blocks of a healthy gut and body.
While analogous in function to the colon, small intestine metabolites can be quite distinct from the fiber-derived metabolites of the large intestine microbiome. Some small intestine metabolites help regulate the upper gut’s production of GIP, a sister molecule to the lower gut hormone GLP-1, which makes up the weight loss and type 2 diabetes drugs Wegovy and Ozempic. Together, with another lower gut hormone called PYY, this triumvirate is critical for coordinating your body’s response to food by regulating your appetite and blood sugar.
Monjaro is an incrementally more powerful combination of GIP and GLP-1 compared with Wegovy and Ozempic. The full complement of these hormones is naturally stimulated by the breakdown of products from both the large and small intestine microbiome.
The upshot on gut breakdown
Research has linked a disrupted small intestine microbiome to diseases of the gut. These include irritable bowel syndrome (IBS), small intestinal bacterial overgrowth (SIBO), Crohn’s disease and Celiac disease.
These diseases are thought to arise partly from disturbances in the way the microbiome breaks down food. Celiac disease, for example, is associated with the small intestine microbiome’s decreased ability to digest gluten. IBS and SIBO are linked to the opposite: the small intestine microbiome’s ability to too readily ferment fibers and sugars.
Foods like wheat, garlic, onion, beans and certain processed products that are high in FODMAPs – a set of fermentable short-chain carbohydrates – have been shown to contribute to symptoms in individuals with SIBO and IBS. Lactose-rich dairy is a high FODMAP food group implicated in lactose intolerance and linked to an overzealous small intestine microbiome.
The body’s not-so-diplomatic immunity
Diseases associated with the small intestine microbiome aren’t limited to metabolism and the gut. In the gut’s lining resides a virtual embassy of immune cells that remain in an ever-vigilant state surveying the motley stream of microbial and nutritional antigens passing through your gut.
Compromise in the security systems that separate the fecal stream from the rest of the body and the processes that keep immune responses in check are hypothesized to play a role in triggering various autoimmune conditions in which the body becomes confused as to who’s friend and who’s foe.
Studies have linked inflammatory changes in the small intestine microbiome to type 1 diabetes, where the body’s circulating immune cells attack insulin-producing cells in the pancreas, and to the extra-intestinal symptoms of Celiac disease, where immune cells can lead to destructive processes in the body’s eyes, skin and joints.
Lights shed in and on the tunnel
Up until very recently, small intestinal research has moved slowly. Scientists relied on upper endoscopy procedures, which involve sedation and inserting a small camera at the end of pinky-thick tubes through the mouth into the very first part of the small intestine.
One of the few alternatives to endoscopies has been studying patients who have had intestinal surgeries that leave direct portals into their small intestine via a hole in their abdominal wall.
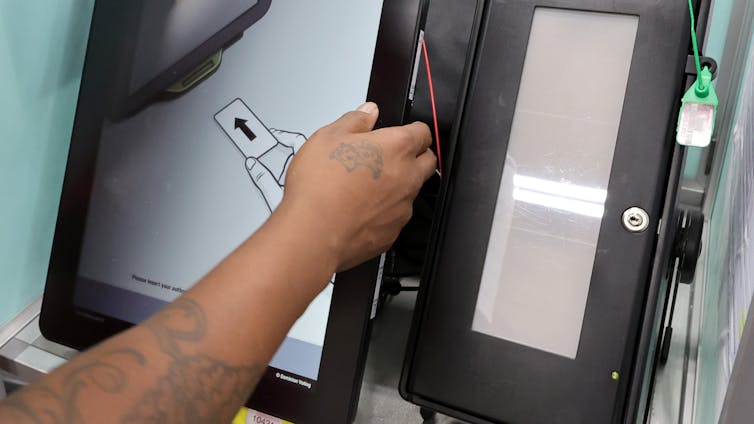
Newly developed technologies are removing the need for sedating medications and unique anatomical situations by allowing scientists to more easily sample the furthest reaches of the gut. Such technologies include camera capsules tethered to angel-hair-thin filaments and other even more streamlined devices that create minimally invasive direct lines of access to the small intestine. Researchers have also developed capsules with sample compartments that open when they reach certain acidity levels in the body.
Improvements in endoscopy techniques are making it easier to study the small intestine.
These new sampling techniques have unlocked unprecedented access to the upper gut, paving the way for new insights and therapies. In a real-life parallel to a childhood favorite, “The Magic School Bus, Inside the Human Body,” researchers can now ride along through the gut like Ms. Frizzle and her class, shining light on the microbial secrets held within.
Accrued alliance in a still-crude science
Therapies based on early understandings of the gut microbiome have included approaches ranging from probiotics to fecal transplants and prebiotics to fermented foods.
But new treatments for gut health are still in their early days. Studying the small intestine could provide insights to improve therapeutic development. A couple of promising future possibilities include partnering small intestine bacteria with their preferred prebiotics and personalized combinations of low FODMAP prebiotics designed to avoid small intestine fermentation.
Treatments that partner food and the microbiome are likely early harbingers of what’s to come in the rapidly developing field of microbiome medicine. Researching the small intestine – and not only the gut’s tail end – might just be microbiome medicine’s most pioneering upstream start.
Christopher Damman, Associate Professor of Gastroenterology, School of Medicine, University of Washington
This article is republished from The Conversation under a Creative Commons license. Read the original article.